Differences Between Type 1 and Type 2 Diabetes
Diabetes is a chronic condition that affects how your body processes blood sugar (glucose). While both Type 1 and Type 2 diabetes involve problems with insulin, the underlying causes and management strategies differ significantly. Understanding these differences can help you better manage the condition or reduce your risk.

Causes and Development
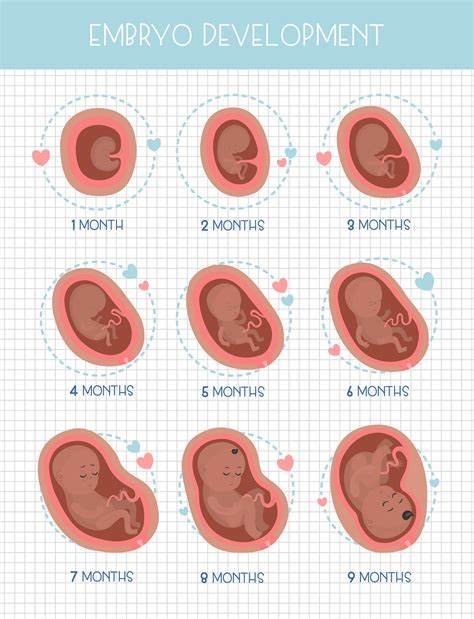
Type 1 Diabetes is an autoimmune condition. It occurs when the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the body can no longer produce insulin, which is needed to regulate blood sugar levels. This type of diabetes typically develops in childhood or adolescence, although it can occur at any age.
Type 2 Diabetes, on the other hand, develops when the body becomes resistant to insulin, and the pancreas is unable to produce enough insulin to compensate for the resistance. Unlike Type 1, Type 2 diabetes is more common in adults, although it is increasingly seen in younger people due to rising obesity rates. Factors such as genetics, age, poor diet, and physical inactivity contribute to the development of Type 2 diabetes.
Symptoms
The symptoms of Type 1 diabetes often develop quickly, over a few days or weeks. Symptoms include:
- Frequent urination
- Unexplained weight loss
- Extreme hunger and thirst
- Fatigue and weakness
- Blurred vision
In Type 2 diabetes, symptoms tend to develop more slowly and may be subtle or even unnoticed in the early stages. Common symptoms include:
- Increased thirst and hunger
- Frequent urination
- Fatigue
- Blurred vision
- Slow-healing wounds
- Numbness or tingling in hands or feet
Age of Onset
Type 1 diabetes is most commonly diagnosed in children, teenagers, or young adults. It accounts for about 5–10% of all diabetes cases.
Type 2 diabetes is more common in adults over 40, though it is increasingly being diagnosed in younger people, especially due to rising rates of obesity and sedentary lifestyles. It accounts for about 90–95% of all diabetes cases.
Insulin Dependence
People with Type 1 diabetes are insulin-dependent because their bodies do not produce insulin at all. They must take insulin injections or use an insulin pump for the rest of their lives to regulate their blood sugar levels.
In Type 2 diabetes, insulin resistance usually develops over time. Initially, many people can manage their condition with lifestyle changes, such as diet and exercise. However, as the disease progresses, oral medications may be prescribed to help the body use insulin more effectively. In some cases, insulin may also be required.
Risk Factors
For Type 1 diabetes, the exact cause is unknown, but genetic factors and an autoimmune reaction play a significant role. It is not typically associated with lifestyle choices.
Type 2 diabetes is more closely linked to lifestyle factors, including:
- Being overweight or obese
- Lack of physical activity
- Unhealthy eating habits
- Family history of diabetes
- Older age
- High blood pressure and high cholesterol levels
Management and Treatment
Type 1 diabetes requires lifelong insulin therapy. People with Type 1 diabetes must monitor their blood sugar levels regularly, adjusting insulin doses based on food intake, exercise, and other factors.
In Type 2 diabetes, the treatment approach often starts with lifestyle changes. Adopting a healthier diet, increasing physical activity, and losing weight can significantly improve insulin sensitivity. If these measures aren’t enough, oral medications may be prescribed to help lower blood sugar levels. In more severe cases, insulin injections may be necessary.
Long-Term Complications
Both types of diabetes can lead to serious long-term complications if not well-managed, including:
- Heart disease and stroke
- Kidney damage (nephropathy)
- Nerve damage (neuropathy)
- Eye problems (retinopathy)
- Poor circulation and amputations
However, Type 1 diabetes tends to lead to complications earlier in life since it often begins in childhood, while Type 2 diabetes typically takes longer to develop complications, but the risk increases over time if left unmanaged.
Conclusion
While Type 1 and Type 2 diabetes share some similarities, such as their impact on insulin and blood sugar levels, they are fundamentally different in terms of cause, age of onset, and management. This is an autoimmune condition requiring insulin from the onset, whereas Type 2 diabetes is primarily lifestyle-related and can often be managed through lifestyle changes and medications. Understanding these differences can help people better manage the condition and make informed decisions about their health.